Objective
Assess the tenderness and resting tone of the pelvic floor at rest;
Assess the strength of voluntary pelvic floor muscle contractions;
Assess the relaxation of pelvic floor muscles following a voluntary contraction;
Determine the need for referral to a licensed pelvic floor physical therapist.
Instructions
Assist the client into a comfortable supine position.
Legs should be comfortably bent at the hips and knees, allowing complete relaxation of legs, hips, buttocks, and abdominal muscles. Use pillows or supports as needed. Ask the client to tilt their pelvis toward the ceiling as necessary. Avoid using “relax” as a command, instead focus on specific ways the client could move or not move in order to stop activating the muscles in their back, buttocks, hips, abdominals, or legs.
Visual inspection of the vulva, perineum, and anus.
Note areas of redness, scar tissue, fissures, and inflammation.
Ask the client to cough while visualizing the perineum.
Normal function: the perineum does not move downward.[1]
Abnormal function: the perineum shows downward movement.
[1] The pelvic floor should spontaneously respond to the increased abdominal pressure from a cough/laugh/sneeze by a well-timed contraction that will stabilize the urethra and support the pelvic organs. A normally functioning pelvic floor contracts automatically without the need for conscious voluntary control (Bo, Stuge, & Hilde, 2019).
Ask the client to bear down (Valsalva maneuver) while visualizing the perineum.
Effective effort: the perineum bulges.
Ineffective effort: the perineum does not move
Digital palpation of the pelvic floor muscles
Use single- or double-gloved finger(s) with generous lubrication (per client’s choice).
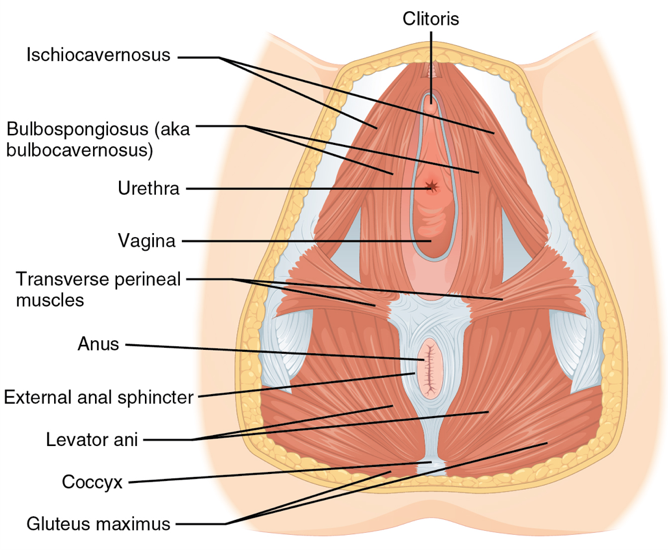
a. Internal palpation of the superficial pelvic floor muscles, including the ischiocavernosus, bulbospongiosus, transverse perineal muscles, and the perineal body. See Figure 1. Assess tension and tenderness at rest.
b. Internal circumferential vaginal palpation of deep pelvic floor muscles, including the levator ani complex and obturator internus (located on the lateral pelvic wall at 3-5 o’clock and 7-9 o’clock positions). See Figure 2. Assess tension and tenderness at rest.
a. Ask the client to contract the pelvic floor muscles around your palpating finger(s).
Do not ask the client to do a “Kegel.” This is a dated and misused term that may or may not accurately translate what the provider is asking the client to do.
Use at least 3 different verbal cues to elicit a pelvic floor contraction. Example verbal cues include:
“squeeze and pull in my fingers”
“stop the flow of urine”
“close the openings and lift up and in”
“bring the ‘sits bones’ together”
“lift a marble up into your vagina”
“bring the pubic bone and tail bone together”
“pretend you’re squeezing around your partner/vibrator/fingers”
“gently draw in your low abdomen”
“hold back gas and hold back a stream of urine”
“wink the anus”
“imagine an elevator rising up in your vagina”
“pretend your vulva is an elevator and close the doors”
b. Determine if the pelvic floor contraction was effective
Effective: visualization of perineum drawn upward and inward without straining from ancillary muscle groups (most commonly the buttocks, hips, legs, and abdominals). An effective pelvic floor contraction uses the pelvic floor musculature to squeeze around the urethra, vagina, and rectum.[2]
Ineffective: straining rather than contraction occurs (assess the use of ancillary muscles in the buttocks, hips, legs, and abdomen), visualization of perineal descent or no visual change.
Assess strength, tone, tenderness, and coordination of contraction and relaxation.
Classify the strength of the contraction as absent, weak, normal, or strong.
Classify the relaxation after the contraction as absent, partial, or complete.
[2] During an effective pelvic floor contraction, the pelvic floor muscles squeeze the urethra against other tissues, resulting in stabilization of the bladder neck and urethra, as well as increased urethral pressure. This combination holds back urine and results in continence (Bo, Stuge, & Hilde, 2019).
Determine the need for a referral to a licensed pelvic floor physical therapist.
a. If the client has abnormal function during the cough test (#3) refer them to a licensed pelvic floor physical therapist.
b. If the client has ineffective effort during the Valsalva maneuver (#4) refer them to a licensed pelvic floor physical therapist.
c. If the client reports pain and/or tenderness with internal palpation of the pelvic floor muscles (#5) refer them to a licensed pelvic floor physical therapist.
d. If the client is unable to do an effective pelvic floor contraction (#6a) refer them to a licensed pelvic floor physical therapist.
e. If the client is unable to completely relax after a pelvic floor contraction (#6b) refer them to a licensed pelvic floor physical therapist.
Figure 1.
Muscles of the female pelvic floor. Reprinted from OpenStax Anatomy and Physiology, OpenStax CNX, 2017, Retrieved fromhttp://cnx.org/contents/14fb4ad7-39a1-4eee-ab6e-3ef2482e3e22@8.108.
Figure 2.
Digital palpation of the deep pelvic floor muscles. Reprinted from “Recognition and Management of Nonrelaxing Pelvic Floor Dysfunction” by S.S. Faubion, L.T. Shuster, & A.E. Bharucha, 2012, Mayo Clinic Proceedings, 87(2), 187-193.